
By Kevin R. Suzuki DMD, MS

Ridge atrophy is well documented and dramatic. This is well illustrated in the prospective study by Schropp et al. which demonstrated changes of an edentulous site after tooth extraction over the period of a year (1). Edentulous ridges were shown to demonstrate an average of 50% loss of buccal-lingual dimension; the majority lost during the first 3 months. Studies by Iasella et al. also document significant changes in apical-coronal dimension of the alveolar ridge post-extraction (2).
The patient’s goals are discussed and which option(s) best suit the situation. In many cases options to replace an edentulous area may include: implant-supported restoration, tooth supported-fixed prosthesis, removable prosthesis, no treatment. Many patients may desire an option to most closely replicate the form, function, and esthetic capacity of the original tooth or teeth. An implant-supported restoration may prove to be the most desired optimal solution. For an edentulous site where there can be a significant compromise to native tissues and inadequate alveolar dimensions (such as a missing tooth for one year or longer), alveolar changes can complicate or rule out the possibility for placement of a dental implant.

Ridge atrophy frequently requires regeneration of oral tissues including preservation of soft and hard tissues in preparation for placement of a dental implant. This concept, called “ridge or site preparation/augmentation” (less appropriately “socket grafting”), has been well detailed in published texts by Suzuki and Misch (3) among a growing body of literature. Ideally this augmentation should be performed at the time of or within 8 weeks after the extraction to ensure preservation of the maximum volume of residual bony ridge.
Clinicians may predict the degree of successful defect regeneration with bone augmentation based upon the number bony walls present (which provide vascular supply and pathways for cells and biologic factors to stimulate regeneration). A four-wall defect is the most predictable (i.e. a completely intact tooth socket) and may not require bone augmentation if allowed to heal undisturbed long enough. One-wall or No-wall defects prove to be the most challenging scenarios providing the least number of vascular walls for reparative and regenerative potential. Augmentation of these defects may involve simple to multimodal techniques that incorporate one or any combination of a materials including: bone graft, cell-occlusive membrane, biologics, tacks, screws or meshwork barriers.
Combination grafting techniques tend to be most predictable when including the principle of guided tissue regeneration by employing an absorbable or nonabsorbable membrane. It is through this principle, well established in wound healing literature by Melcher, that regeneration of bone around compromised teeth with bony wall defects has been shown to promote reattachment of the periodontal ligament and regrowth of alveolar bone (4). This technique is also successful for extraction sockets.
When considering what types of graft materials are best to use for ridge preservation the clinician should consider what ideal material characteristics are most appropriate: absence any risk of immune rejection by the recipient, predictable long term preservation of the bone in the edentulous site, working ease. It has become commonly recommended to implement the following hierarchy when considering appropriate bone augmentation materials for implant site development:

Autogenous
Human derived allograft
Bovine, Porcine or Equine xenograft
Alloplast
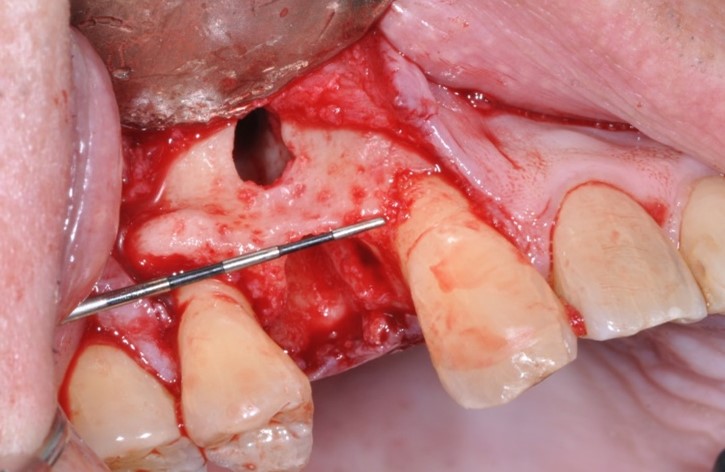
Barrier membranes exclude surrounding, faster growing epithelium cells from populating an extraction socket allowing bone remodeling, deposition, and maturation. The addition of bone augmentation material acts as an osteo-inductive and/or osteo-conductive scaffold. Angiogenesis of new blood vessels into the site promote introduction of osteoprogenitor cells. These osteoblasts and osteoclasts utilize the mineral components of the graft material to deposit organized, osseous architecture over a period of three to six months. Angiogenesis can be enhanced with decortication of the existing bony architecture allowing enhanced bulk and density, a principle called “regional acceleratory phenomenon”.

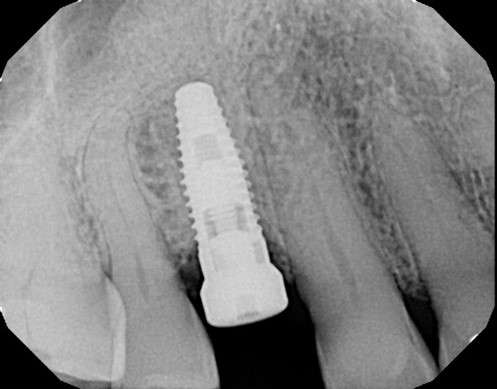
After healing and maturation of the graft to turn over into native bone, dental implant therapy can be predictably implemented and an implant body positioned for the ideal restorative position. Implant dentistry has moved away from the historical approach of placing an implant body where the bone is most favorable. The paradigm has emerged where implant treatment plans should be driven from a “restoration driven” approach. The design of implant restoration and implant body position is dictated by the ideal prosthetic position.
Due to advances in CT scanning technology, reduced costs, and improved CT scan access the osseous architecture of a proposed implant site can be pre-operatively evaluated. Treatment plans may be determined and predict whether augmentation may be indicated in an edentulous site. If it is identified that there is not enough bone or it is not in the correct position to place an implant it is better to rehabilitate the ideal alveolar ridge form first. This will permit ideal implant placement in the most appropriate prosthetic position to restore without compromise or likelihood of increased stress or restorative shortcoming in the design of the implant-prosthesis system. As dental treatment plans continue to support patients’ clinical objectives for dental implants, ridge preservation and bone grafting following tooth extraction becomes a critical component of implant site preparation. Clinical outcomes are more predictable and successful with a basic understanding of the fundamentals of bone grafting and guided bone regeneration.

Conclusions: It is proposed to offer, as a standard of care, ridge preservation of extraction sockets and treatment planning for the option of future dental implant(s). Sound clinical research supports these patient therapies.
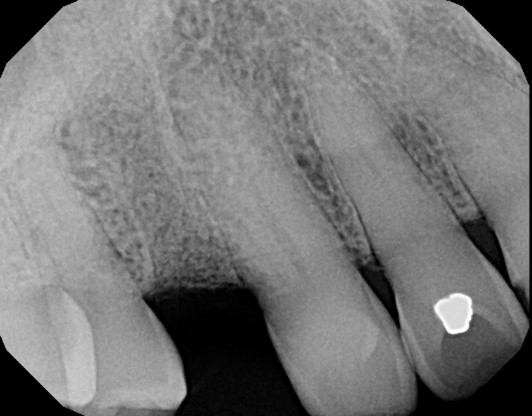
Figure Legend: A 38 y.o. white male patient presented with a chief complaint of persisting pain in the upper right area, ( tooth #5) for days. Diagnosis was endodontic lesion with a hopeless prognosis (Figure 1, 2). The tooth was extracted and Regional Acceleratory Phenomena performed (Figure 3), grafted with Allograft and Resorbable membrane (Figure 4 &5) employed for Guided Bone Regeneration (GBR) and sutured (Figure 6). Four months post Extraction and Ridge Preservation surgery (Figures 7 and 8, Implant was placed (Figure 9) to be restored after osseointegration period.
Acknowledgements: contributions and support from Jon B. Suzuki DDS, PhD, MBA
Conflict of interest: Dr. Suzuki works as a consultant for Millenium Dental Technologies
References
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Perio Restor Dent. 2003; 23(4):313-23.
- Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-9.
- Misch CE, Resnik RR, Suzuki JB, et al. “Tooth Extraction, Socket Grafting, and Barrier Membrane Bone Regeneration.” Contemporary Implant Dentistry 4th ed. St. Louis: Mosby Elsevier, 2020. 870-904.

Dr. Suzuki will speak on this topic at the 2024 Florida Dental Convention on June 20-22 in Orlando. You can find more information on his courses at www.floridadentalconvention.com.
